HAZLETON, PA - Federal inspectors found multiple deficiencies at The Pavilion at St Luke Village nursing home during a July 2024 survey, including a nearly two-month lapse in infection prevention monitoring, incomplete documentation of a resident-on-resident altercation, and failure to coordinate hospice care services for a terminally ill resident.
Infection Prevention Program Halted for Nearly Two Months
The most significant finding from the July 19, 2024 inspection involved the facility's complete failure to maintain its infection prevention and control program for approximately eight weeks during June and July 2024.
According to the inspection report, the facility's infection control surveillance and data analysis activities ceased after May 27, 2024. During the survey, inspectors found no documented evidence that the nursing home was monitoring, investigating, analyzing, or managing healthcare-associated infections from late May through mid-July.
The gap in oversight occurred when the facility's Infection Preventionist, identified as Employee 6, transitioned to a different role on June 5, 2024. When interviewed by inspectors, she confirmed she had coordinated and implemented the infection control program until that date but was unable to provide any evidence of surveillance activities after May 27, 2024.
The Nursing Home Administrator confirmed during an interview on July 19, 2024, that the Infection Preventionist was not performing the required duties and that the facility had failed to fully implement a comprehensive infection monitoring program for the two-month period in question.
Why Infection Surveillance Matters in Nursing Homes
Nursing home residents face significantly elevated risks from infectious diseases due to several factors: advanced age typically weakens immune system function, chronic medical conditions further compromise the body's ability to fight infections, and the congregate living environment creates conditions where pathogens can spread rapidly from person to person.
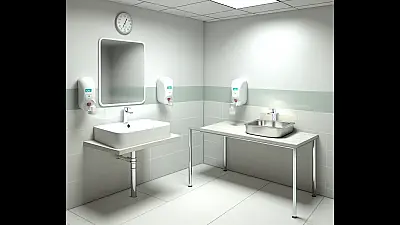
Infection prevention programs serve as an early warning system for healthcare facilities. By systematically tracking infections, facilities can identify outbreaks in their earliest stages, recognize when unusual pathogens are present, and detect trends that might indicate problems with sanitation, hand hygiene compliance, or other preventive measures.
The facility's own policy, reviewed by administrators on May 9, 2024, states that surveillance tools are used for "recognizing the occurrence of infections, recording their number and frequency, detecting outbreaks and epidemics, monitoring employee infections, monitoring adherence to infection prevention and control practices, and detecting unusual pathogens with infection control implications."
Without active surveillance, a facility cannot detect infection clusters or increases in infection rates in a timely manner. This means that an outbreak affecting multiple residents could go unnoticed for days or weeks, allowing continued transmission before interventions are implemented.
Common nursing home infections include urinary tract infections, respiratory infections including pneumonia and influenza, skin and soft tissue infections, and gastrointestinal illnesses. Each of these can cause serious complications in elderly residents, including hospitalization and death. Early detection through systematic monitoring allows facilities to implement isolation precautions, adjust antibiotic treatments, and identify the source of transmission.
The two-month gap documented at The Pavilion at St Luke Village represents a significant breakdown in a fundamental safety system. During this period, the facility was essentially operating without the ability to systematically identify or respond to infection trends among its resident population.
Physical Altercation Between Residents Not Documented in Medical Records
Inspectors also cited the facility for failing to maintain accurate and complete clinical records related to an incident involving two residents on July 9, 2024.
According to a facility incident report reviewed during the survey, Resident 35 reported to staff that Resident 87 had entered her room uninvited and slapped her in the face. The incident occurred at approximately 4:30 PM when Resident 35 told Resident 87 to put down an orange she had picked up.
Resident 35 had been admitted to the facility with diagnoses including spinal stenosis and hypertension. Resident 87 had been admitted with a diagnosis of Alzheimer's disease.
Despite the incident being recorded in the facility's internal incident reporting system, inspectors found no documentation in either resident's clinical medical record regarding the intrusive wandering or the reported physical altercation.
The Nursing Home Administrator confirmed during an interview on July 18, 2024, that there was no documented evidence in the clinical records of either resident related to the incident.
The Critical Role of Medical Documentation
Complete and accurate medical record-keeping is a cornerstone of quality healthcare delivery. According to the American Nurses Association Principles for Nursing Documentation, nurses must document their work and outcomes to provide the healthcare team with the information needed to ensure informed decisions and high-quality care.
When incidents occur between residents, documentation in medical records serves multiple essential purposes. For the resident who was struck, medical records should reflect any injuries observed, assessments performed, and follow-up care provided. This documentation ensures that subsequent caregivers are aware of the incident and can monitor for delayed symptoms or psychological impacts.
For residents with cognitive impairments like Alzheimer's disease, documentation of behavioral incidents is equally important. These records help the care team identify patterns that might indicate changes in the resident's condition, evaluate the effectiveness of current interventions, and adjust care plans to reduce the risk of future incidents.
Pennsylvania's State Board of Nursing regulations require registered nurses to document and maintain accurate records. The regulations specify that nurses must carry out actions that promote, maintain, and restore the well-being of individuals and are fully responsible for all actions as licensed professionals.
The absence of documentation in this case means that critical information about a safety incident was not communicated through the standard medical record system. Other nurses and healthcare providers caring for these residents would have no indication in their charts that the incident had occurred, potentially affecting their ability to provide appropriate care and supervision.
Hospice Care Coordination Deficiency
A third significant finding involved the facility's failure to properly coordinate care for a terminally ill resident receiving hospice services.
Resident 84 was admitted to the facility with a diagnosis of malignant neoplasm (cancer) of the liver and bile duct. On February 5, 2024, a physician order was placed for the resident to begin receiving hospice services at the facility.
When inspectors reviewed the resident's care plan during the July survey, they found that it failed to reflect coordination of services between the facility and the hospice agency. The care plan did not address how the facility and hospice provider would work together to meet the resident's daily care needs or the specific needs related to the terminal diagnosis.
The Nursing Home Administrator confirmed on July 19, 2024, that the resident's care plan was not coordinated with hospice services.
Understanding Hospice Coordination Requirements
When a nursing home resident elects hospice care, two organizations become jointly responsible for the resident's well-being: the nursing facility continues to provide room, board, and general nursing care, while the hospice agency provides specialized end-of-life services including pain management, symptom control, and emotional support.
Federal regulations require that these two entities coordinate their services to ensure the resident's needs are met comprehensively. This coordination must be documented in the resident's care plan, which serves as the roadmap for all caregivers involved in the resident's treatment.
For residents with terminal cancer of the liver and bile duct, common symptoms requiring coordinated management include pain, nausea, fatigue, and changes in mental status. Without proper coordination, there is risk of duplicated services, gaps in care, conflicting treatment approaches, or delays in addressing symptom changes.
A coordinated care plan should clearly delineate which organization is responsible for each aspect of the resident's care, establish communication protocols between facility and hospice staff, and ensure that the resident's wishes regarding end-of-life care are documented and honored.
The lack of documented coordination at The Pavilion at St Luke Village meant that the care plan did not provide clear guidance on how the facility and hospice agency would work together to address this resident's complex needs during a vulnerable period at the end of life.
Additional Issues Identified
The inspection revealed violations in the following regulatory areas:
- Medical Records Standards (F0842): The facility failed to maintain clinical records in accordance with accepted professional standards, specifically related to the undocumented resident altercation incident involving Residents 35 and 87.
- Hospice Services Coordination (F0849): The facility did not ensure proper coordination of care and services between the facility and the external hospice agency for Resident 84.
- Infection Prevention and Control (F0880): The facility failed to provide and implement an infection prevention and control program, with surveillance activities absent for June and July 2024.
Regulatory Context and Standards
The violations cited during this inspection fall under both federal Medicare and Medicaid certification requirements and Pennsylvania state regulations. The relevant Pennsylvania codes include:
- 28 Pa. Code 211.12: Requirements for nursing services - 28 Pa. Code 211.5: Medical records requirements - 28 Pa. Code 211.10: Resident care policies - 28 Pa. Code 201.21: Use of outside resources
Additionally, Pennsylvania's State Board of Nursing regulations under Title 49 establish documentation and care standards that registered nurses and licensed practical nurses must follow when providing care in long-term care settings.
Facilities found to be out of compliance with federal certification requirements must submit plans of correction explaining how they will address each deficiency and prevent recurrence. The severity of citations can affect a facility's Medicare and Medicaid reimbursement rates and, in serious cases, can result in civil monetary penalties or other enforcement actions.
The Pavilion at St Luke Village is located at 1000 Stacie Drive in Hazleton, Pennsylvania. The inspection was completed on July 19, 2024.
Full Inspection Report
The details above represent a summary of key findings. View the complete inspection report for Pavilion At St Luke Village, The from 2024-07-19 including all violations, facility responses, and corrective action plans.
💬 Join the Discussion
Comments are moderated. Please keep discussions respectful and relevant to nursing home care quality.